"Universal Masking" & Coronaphobia in Hospitals & Healthcare *Also* Screws up Medical Teams
An obvious corollary to some under-appreciated research on mask-wearing
I’ve written at length (here, here, and elsewhere) about how universal masking policies can be a special kind of hell for the particular population seen in long-term care (LTC) facilities.
Briefly, according to very large-scale estimates, between 60-70% of your typical LTC residents have “clinically meaningful” hearing loss1 - typically defined by the inability to reliably perceive a noise lower than <40 DB (which is about the noise of most casual, quiet conversation).

Not only that, according to generally accepted figures, somewhere in the neighborhood of 50% or more of average USA long-term care residents have a diagnosis of major neurocognitive disorder - or what’s more commonly referred to as dementia (like Alzheimer’s Disease).
With that, of course, comes even more significant challenges these people face in their daily lives in terms of communicating with, and perceiving the world around them.
Basically, with a population where deafness and dementia is rampant, constantly masking and muffling the faces of caregivers, family, and whatever residents will comply basically guarantees increased confusion, depression, and behavioral problems. Like I’ve said before - for nursing home residents, masks are a prison within a prison.
So, very smart - let’s *constantly* mask everyone that lives around these poor people, right?
The Effects of “Universal Masking” on Healthcare Staff
One of the ways that universal masking can lead to medical errors is through communication barriers. Masks can muffle speech, making it difficult to hear and understand instructions or important information during patient handoffs or in critical situations. This can lead to misunderstandings and errors in patient care.
Here are some of the often subtle issues that “universal masking” causes amongst teams:
"Facial expressions are a vital aspect of human communication, conveying information that cannot be expressed through language alone. Our ability to interpret these expressions is so deeply ingrained that we often do it subconsciously, without even realizing it." - Mark Changizi, Ph.D.
Getting rid of the lower half of the face eliminates a huge source of what is in effect several hundred thousand years of evolutionary adaptation - facial expressions - that provide important contextual cues to help supplement verbal interaction amongst teammates. This then makes language more ambiguous. We may need to ask our colleagues to repeat themselves & elaborate more. This takes precious time and in critical situations in medicine, this may be time that cannot be spared.
Reduces team cohesion. Our medical director likes to tell goofy jokes and then has a silly look on her face when she waits for us to ‘get’ the punchline. We all relax when our longtime nurse admin lets out her big belly laugh when our medical director tells one of her dumb jokes. Masks depersonalize us as teammembers. We work less effectively. There’s more distance between us.
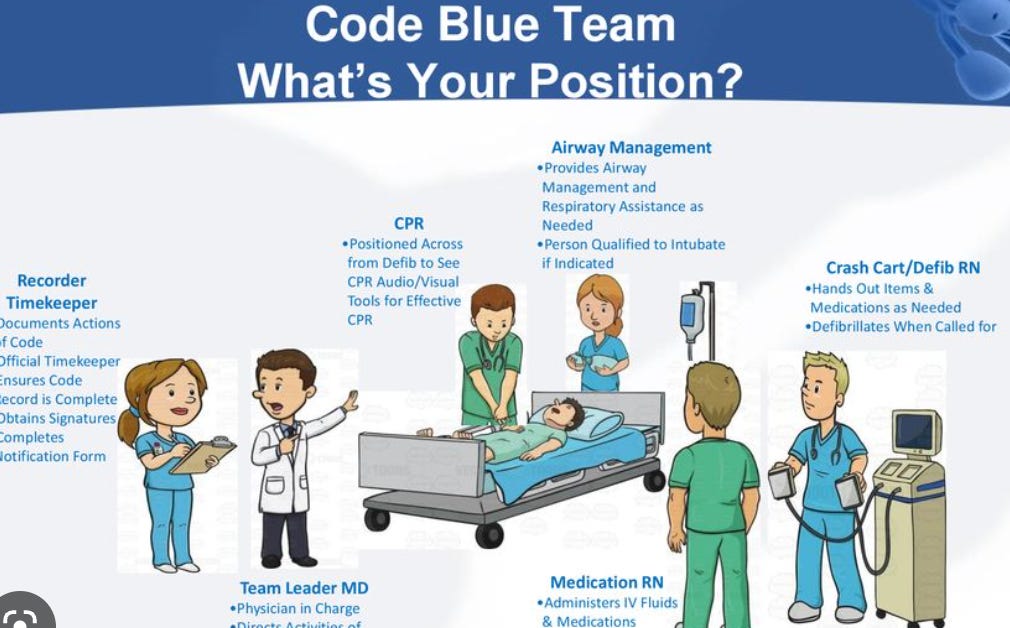
Although I’m in long-term care, we do have our emergency situations, like quickly evaluating residents for injuries from falls, or tending to potential medical crises like chest pain, respiratory distress, or occasionally, a “code blue” situation, where a resident requires CPR. In all of these cases - it’s critical that team-members are able to seamlessly and directly communicate with each other. Yet, excessive PPE use in these situations causes healthcare personell to function less well, with a potentially reduced field of view, poorer communication between teammembers, more cognitive exhaustion, poorer thermoregulation - all potentially impacting performance of clinicians.2
Like any inpatient environment, nursing homes can be high-stress, with residents who suffer from dementia (often with behavioral problems because of it), and at times we have unpredictable, emergency situations and a critical need for high team cohesion.
Masking up everyone on the healthcare team, particularly with N95s, faceshields, and gloves, is going to be cause more medical errors (obviously the question for us is - is it worth it as a “universal” measure, in any form?).
Communication gets impaired: Communication is a critical aspect of team functioning in ALL healthcare settings, and the use of masks complicate. Masks muffle speech, making it harder to hear and understand what others are saying, *especially* in noisy environments like an ER. Masks can also obscure facial expressions, which can be important for conveying emotions and building trust between team members.3
It contributes to an environment of decreased trust: Trust is essential for effective teamwork, and the use of masks can decrease the level of trust between team members. When team members cannot see each other's faces, it can be harder to read nonverbal cues and develop a sense of mutual trust and respect.
Reduced collaboration: Collaboration is important for ensuring that all team members are working towards the same goal and are able to share their expertise and perspectives. The use of masks can make it more difficult to collaborate effectively, especially in situations where there are language barriers or other communication challenges.
The Story of Joyce, our Belly-Laughing Nurse Administrator
Let’s shift focus a bit. What about us healthcare professionals who *take* *care* of our residents?
One of our nurse administrators - I mentioned her before - let’s call her Joyce. Joyce is one of the finest admins we’ve had at our nursing home. She’s started years and years ago as a med nurse, then RN, and eventually got promoted to assistant, then a few years ago, right before COVID, as one of the two chief nurses for our two units in our facility.
She’s a great nurse as well as a great teammember. She always gets along with her counterpart from the other unit, shows up regularly at our care plan meetings, but also takes the time to meet personally with our residents (she started as a floor nurse here - and never seems to be able to let it go).
Unfortunately, and we’ve all known this about Joyce for some time - she has hearing loss, and wears hearing aids.
Since COVID started, Joyce has been seen more often than not with one of the four assistant chief nurses, and at times has had me accompany her for key meetings with certain residents - not for clinical reasons, but because Joyce can’t understand what people are saying nearly as much any more.
I see Joyce struggle. With phone calls, and patient contacts. I’m shocked she hasn’t retired yet. I try to help her when I can.
We all do. She’s a great admin. But we’ve all seen that the “universal masking” rules have been particularly tough on her.
They’ve been tough on all of us.
The problem I have with it - I don’t think it really ended up accomplishing anything other than hurting patients and alienating us all from each other.
Reed, N. S., Altan, A., Deal, J. A., Yeh, C., Kravetz, A. D., Wallhagen, M. I., & Lin, F. R. (2018). Trends in health care costs and utilization associated with untreated hearing loss over 10 years. JAMA otolaryngology-- head & neck surgery, 144(9), 763-765.
Ruskin, K. J., Ruskin, A. C., Musselman, B. T., Harvey, J. R., Nesthus, T. E., & O'Connor, M. (2021). COVID-19, Personal Protective Equipment, and Human Performance. Anesthesiology, 134(4), 518–525. https://doi.org/10.1097/ALN.0000000000003684
“Verbal communication through masks can be difficult, with speech muffled or completely inaudible, especially for those with thick accents or speaking quietly. Additionally, nonverbal communication, such as facial expressions, may be obscured or eliminated entirely, making it more difficult for team members to interpret cues from one another."
- in James, John T. PhD. A New, Evidence-based Estimate of Patient Harms Associated with Hospital Care. Journal of Patient Safety 9(3):p 122-128, September 2013. | DOI: 10.1097/PTS.0b013e3182948a69





As an audiologist who works with primarily adult patients, especially the elderly, masking has had a huge negative impact on communication. There are a few of my patients who (for whatever reason) will not wear hearing aids and masking makes it virtually impossible for them to communicate. They have withdrawn socially as well and I shutter to think what they miss especially at medical appointments (where they often are alone). Enough of the masking nonsense in a standard medical clinic. It needs to stop. The harm it is doing is significantly more than the protection it is supposed to be providing. Sadly, at least in my clinic, until the CDC says to stop, my bosses will continue the charade.
It’s so frustrating that healthcare, of all places, thinks it essential to continue masking. The fact masks have done nothing combined with harms, makes their use a net negative. Thanks for so eloquently highlighting one of the not often thought of harms: medical errors.