Re-Imagining Long Term Care
The current system of LTC in the USA - centralized & subservient to heavy-handed government control - has prevented localized experimentation in various, pro-quality-of-life care philosophies.

A few weeks back I remarked on my friend Hal Cranmer, who runs a fantastic small chain of assisted living facilities in the Arizona area. He tweeted the following:
Of course, he’s correct.
Both Hal and I are in agreement that the way that eldercare is typically funded & regulated in the USA tends to significantly disincentivize innovation.
Yes - of course, the regulations in this space were intended for very noble things (as I noted), to address some of the very well-publicized instances of patient abuse & neglect, use of physical restraints on dementia patients, and overuse of harmful medications in care homes that sprouted up and grew like topsy after the US began directly funding long-term care with federal dollars (administered by states via the Medicaid program) in 1965.

In LTC, we are under the maximum amount of centralized control by federal authorities, with nearly 2/3 of our funding coming from government sources, primarily Medicaid (and if we take Medicaid - we are required to abide by the regulations promulated by CMS, e.g., the Centers for Medicare and Medicaid Services).
Assisted Living Facilities like Hal’s by contrast, are (at least for now) still funded primarily by out-of-pocket, private pay.
There are Care Philosophies in of Long Term Care that are Humane, Innovative, and Different
Regardless, there have been experiments in long-term care that have taken place over the years. I wanted to highlight a few that I have always been excited about (but these days seem to be sketching out ideals that are as far away as ever):
Eden Alternative is a nonprofit founded in the 1990s by geriatrician Bill Thomas, who was working as a nursing home director & saw a need for a model of long-term care that was more humane and focused on quality of life in residents, and to promulgate training and resources to nursing homes that want to emphasize his model.
I’ve consulted at a few nursing homes when I was younger that explicitly took pains to do an “Eden Home” inspired take on care, and I remember one in particular: it was filled with paintings and artwork, there were caged songbirds in the two common areas that nursing staff fed, and all over the nursing home (interestingly, given the songbirds) were cats.
One of the very happy images in my mind from my time consulting at this particular home was one resident who I briefly met who was largely bedbound, but never seemed to be too distressed - and always had a cat sleeping on his bed, keeping him company.
Also a brainchild of Bill Thomas is the Green House Project care philosophy - while Eden Homes focus specifically on aesthetics and “culture change” elements of nursing staff designed to provide a more person-centered (as opposed to traditional, disease-centric approach) to care, this philosophy is focused on creating small, self-contained homes (AKA “small homes” or “neighborhoods”) that each house 10-12 residents.
These self-contained “neighborhoods” are designed to be more homelike, with private bedrooms and bathrooms for each resident, and a communal living room and kitchen. The focus is on creating a more intimate and familiar environment for residents and promoting a sense of community among residents and staff. It complements the Eden Alternative approach by focusing much more on the living space, the actual physical environment of care itself.
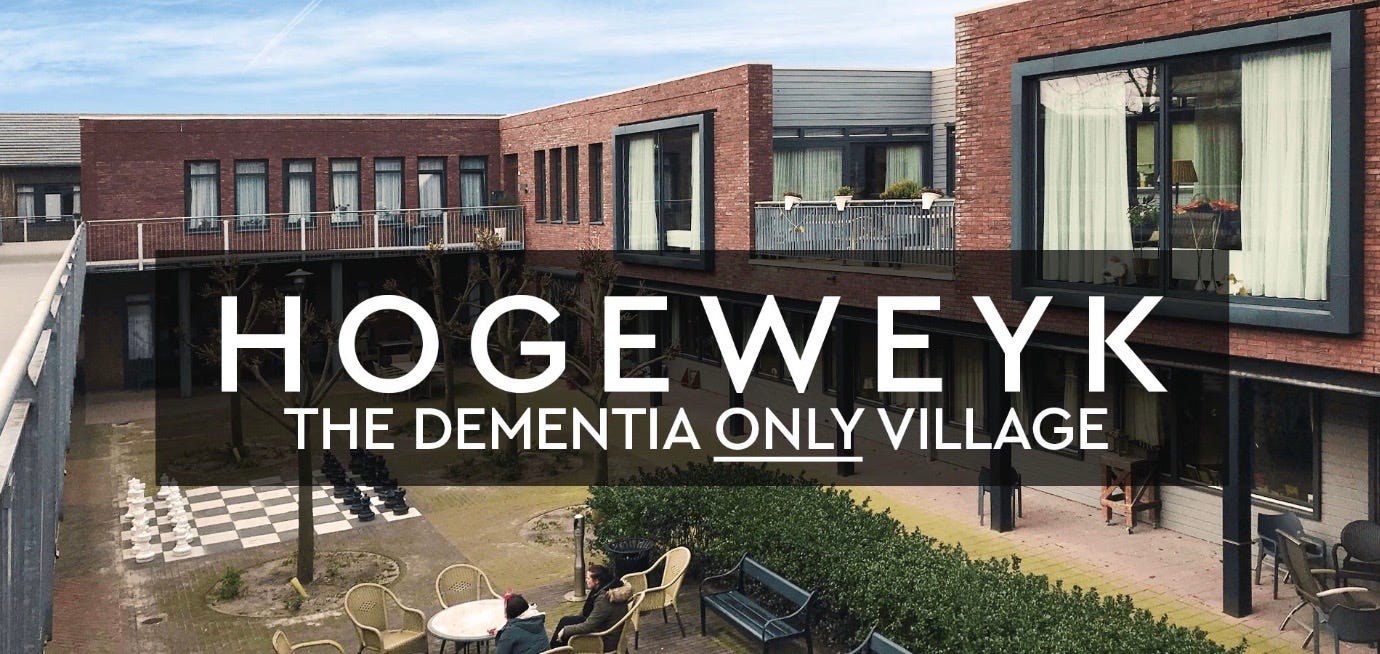
Focusing in particular on the memory care aspect of long term care is one of the most innovative approaches I’ve seen thus far, the dementia village concept, which creates a community within a community - but instead of the much more stark, traditional institutional contours of facility care that we are familiar with in the United States, the dementia village instead places their memory-impaired residents in deliberately-designed environments designed to comfort the residents, by melding with their sense of the familiar.
The “village concept” to me is one of the most radical, humanized, and beautiful models of facility-based care I can possibly imagine.
There’s a few YouTube videos about this particular model Dutch dementia care facility, I recommend you look them up.
I think it’s wonderful. I think this is what a civilized society does with it’s elders.
The Reality
The reality is that most nursing homes in the United States are currently variations on this theme:
They’re hospitals, basically. Even though they’re supposed to be basically places where the old and infirm go to live out their lives with greater medical supervision than, say, assisted living or “aging in place” at home - they are “nursing homes,” and as I discussed in a previous article, the hospital-like design of nursing homes really is as much a historical accident as much as they are a lack of imagination.1
So here we are.
And the fact is - I think we’re at a point where the prospect of a meaningful, widespread resurgence of a “person-centered care” movement in nursing homes in the Western world is further away than ever.
The COVID pandemic - or what I like to call, the Great Coronaphobia of the 2020s, set back any of the meaningful reforms in the LTC industry by decades, in my opinion.
Is it a Conspiracy to Destroy Long-Term Care?

I’m not a conspiracy theorist by nature - honestly.
But I recognize that facility-based care in the United States is expensive. I also recognize that subsidized government funding has greatly crowded the space over the last 75 years. Regarding that - I also recognize that the USA has almost no balance sheet capacity left.
We’re running out of money. Not cash - that can ultimately always be printed:
But that’s not the same thing as true wealth, a store of capital that can be deployed to our collective well-being, something I explored in a previous article on “The Coming Financial Storm.”
Bottom line - nursing homes and facility-based care are largely in a somewhat accelerated terminal decline.
Quality, facility-based nursing or assisted-living care continue to be prohibitively expensive for all but the most wealthy of private pay consumers.
If you’re forced to send your loved one to a facility, and you have no means - despite the promise of continued regulation by our government overlords, your public options will be of increasingly poor quality.
This means that we will likely return to primarily depending on what we did in the United States prior to the 1940s, when it came to elder care.
Family caregivers.
The 1935 Social Security Act, the 1946 Hill-Burton Act, the establishment of Medicare, and the OBRA Act of 1987 all have served to formalize and expand the medicalization of eldercare in the United States, specifically in terms of our reliance on facility-based care. A good overview on it can be found in this 2009 article in Geriatrics and Gerontology International.









It is within the nature of financial capitalism (I stress financial) to treat its members of the society primarily as consumers, NOT as citizens. Therefore, it makes sense that life in long term care land is a good life only for the most wealthy of private pay consumers. In addition, the modern philosophy of post progressive, trans humanism coupled with climate change has elements of eugenics. iI you are productive, then you are OK, if you cease, then bye bye. There are too many people on earth, so.... Isn't it interesting to read more and more geriatrics writing that the best age to die is 75. After, it is only downhill. Thank you for another great reflexion.
We judge a society on how it treats its (not it's) elders.