What have we done to US nursing homes in the name of COVID lockdowns?
Showing you how COVID mitigation is done in US skilled nursing facilities.
Hello there.
I’m a geriatrician and I work in a medium sized nursing home somewhere in the United States. I also want to keep my job, not get into trouble, but also speak freely – so I’m choosing to publish this Substack blog anonymously. My plan is to publish more regularly on what it actually is like to live in a US nursing home as a resident, now two-plus years into the COVID-19 pandemic and associated, society-wide mitigation measures.
Enjoy.
So - one thing is for certain – when it comes to the question of what is ubiquitously known of now as pandemic lockdowns (e.g., society-wide, government-ordered mass shutdowns of schools, so-called “non essential” businesses, and imposition of mask mandates, etc. – also known as “non pharmaceutical interventions, or NPIs) there seems to be a true consensus as to why they were justified. When I say “true consensus” – I don’t mean the artificially-astroturfed consensus of the Twitter “blue checkmarked” experts, the Risa Hoshinos, Gavin Yameys, and Leana Wen’s of the world – I mean actual, true consensus.
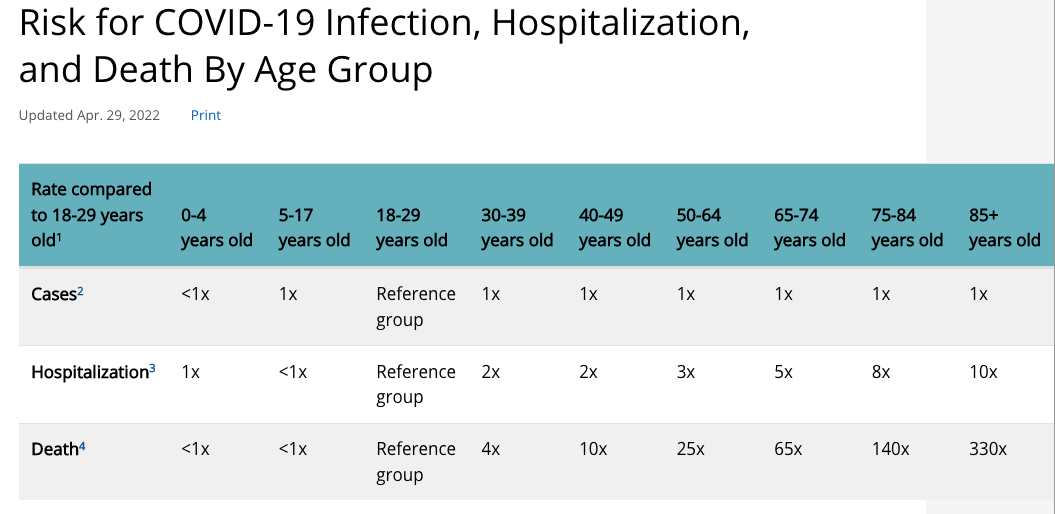
The consensus is as regards the question of older adults. This makes obvious, intuitive sense to even the least educated and non-medically-savvy amongst us. Unless you’ve lived under a rock for the last 2+ years you’re completely aware that the most basic measure of risk related to catching COVID-19, is, well - the risk of dying. Overwhelmingly, the risk is sharply age-stratified, in other words – the older you are (particularly after the age of 70) the more likely it is you are to die from a COVID-19 infection.
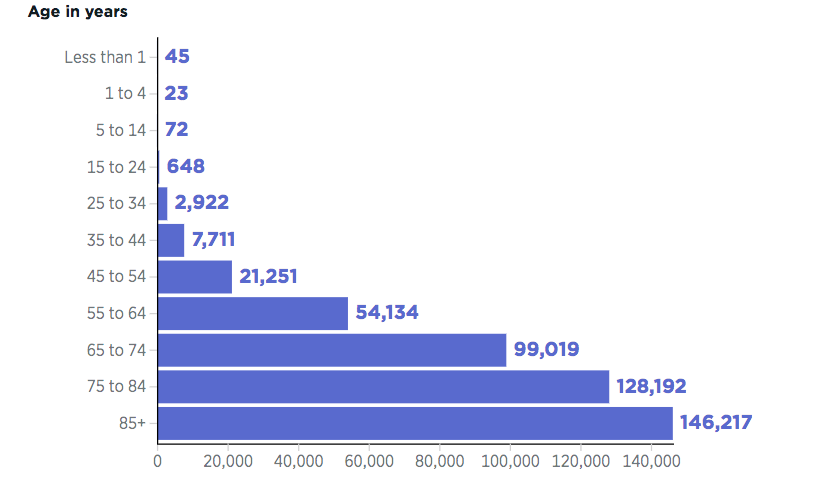
(chart from https://datavisualizations.heritage.org/public-health/covid-19-deaths-by-age/)
The chart above is CDC data, as current as I could find it (February 2021) in a helpful bar-graph format. Another way to visualize the age-stratified nature of COVID-19 risk is as follows:
Basically, the message should be obvious: your risk of dying from COVID-19, if you’re over the age of 60, is somewhere between 25 to 100 times bigger than those of healthy twenty-somethings, and between 100-300 times bigger if you’re over the age of 70.
So what does this mean?
First of all, it means that if you’re a young person or a child – all of the societal energy spent on mandating masks and whatnot for this group is of dubious benefit given the clearly vanishingly small overall risk COVID infection is for them.[1]
Second, it means that if you’re an older adult (say, over the age of 70), you need to give serious thought to the idea that you should be doing more than just, say, getting vaccinated for COVID and then going on your merry way. After all, we’re all pretty aware at this point that in contrast to the rosy “90% effectiveness” of COVID vaccination that was claimed early on, and the claims of authorities like CDC Director Tony Fauci that COVID vaccination would prevent / stop COVID transmission, the actual truth is that COVID vaccinations are much more modestly effective and actually provide no meaningful protection against contracting the virus itself or of slowing or stopping transmission. That being said – they *do* seem to help somewhat, and if you’re in a high-risk group (e.g., such as older adults) I’d say it’s a no-brainer to get one.
The question then becomes, what else do you do?
I work in a nursing home. All of our residents are vaccinated and at this point, triple-boosted. Like many long-term care facilities, we suffered a COVID outbreak, in our case in late 2020, wherein about a dozen-and-a-half of our residents contracted the virus. Two subsequently ended up dying shortly after contracting the virus, giving us an infection fatality ratio of approximately 12.5%, which is on the high side for skilled nursing facilities, but certainly not outside of the norm.
Since then, we have had no further outbreaks at our facility. While we’ve had some occasional staff member testing positive here and there, because of our twice-weekly surveillance testing protocol amongst the staff, we’ve been able to identify the positives amongst staff quickly and pull them off of nursing detail. From the perspective of virus avoidance – we’ve done well since then.
Along with twice-weekly surveillance testing of staff, at my nursing home we’ve done a number of other things that have drastically changed the lives of our residents in the name of virus avoidance.
These are the measures we’ve taken (and these are just the ones I can remember). Italics are my comments.
Our residents no longer dine communally three times per day. They now dine in their rooms.
Not only does this cut off our residents from a prime source of social activity, it also puts them at increased risk for choking due to the lack of centralized monitoring by nursing staff.
Family members, who prior to the pandemic were allowed to visit basically whenever they pleased, day or night, and stay as long as they wanted, are now limited to two-hour, prescheduled visits.
Visitors, of course, need to be masked and show proof of vaccination. If they are unable to show proof of vaccination they are required to show proof of a negative test.[2]
This means that small children (<5 year olds) and babies, who aren’t eligible to be vaccinated and aren’t likely to comply with a COVID test, are still barred from seeing their older adult relatives.
For most of the last 2+ years we have largely banned volunteers from coming into the facility.
Note that this rule has been relaxed somewhat recently, and we’ve had a few bingo games and other events run by volunteers. But – the number of visits and events by volunteers in our nursing home are still far below what they were pre-pandemic, and shutting out our volunteers for two weeks every time there is a positive test result amongst our employees has basically strangled the ability of volunteer services to penetrate our facility in any significant way.
“Paid companion” services have been banned as well (e.g., such as Visiting Angels and other comparable services.
Our residents no longer have access to in-person religious services from our chaplaincy staff. Residents can attend church services via closed-circuit television only, and access in-person visits from our chaplain on demand.
All of our residents, for the last 2+ years, have not been allowed to leave our facility, except for approved outside medical appointments.
That means no more weekend visits or overnight visits with family. No more movie outings with our activity staff, no more restaurant visits, no more going out to dinner or lunch with family in town.
Our residents are not even allowed to amble around the front area of our nursing home, or tool their motorized wheelchair outside to go “on a stroll” (e.g., to birdwatch, or what have you). They can only be outside on our two outdoor patios.
Finally – all staff are required to wear surgical masks and eye protection such as face shields – although recently that has been relaxed so that staff can at least wear eye protection (like carpenters goggles) in lieu of the shields. Note – all residents are “required” to wear masks as well, but in practice we really just “strongly encourage” it – as it’s difficult to get our residents with dementia to do anything consistently.
Regarding mask-wearing, estimates are that between 50-70% of nursing home residents in the United States suffer from some form of diagnosable dementia (e.g., Alzheimer’s Disease, vascular dementia, etc). Moreover, sensory loss such as deafness are rampant in this population. That being said – this is a population that is extraordinarily sensitive to impediments to communication and really need all the help they can get to understand – and to be understood by others. It’s undeniable – mask-wearing muffles clinicians and family members, and cuts off the hearing and cognitively impaired from the ability to read lips and fully read facial expressions – which only serves to confuse our population further and cut them off from communication more.
Regarding not being allowed to leave – this just goes along with the other stuff, the fact that residents in nursing homes now are essentially virtual prisoners.
They are isolated from the world, sealed off.
They cannot be visited unless you are behind masks and face shields / goggles. They are not allowed to leave (unless they discharge – which if you’re a nursing home resident, is not a casual thing).
They are discouraged from socializing with other residents and functionally and practically discouraged from socializing with family.
They are not allowed to see their great-grandchildren. They are not allowed the simple pleasure of going to a movie theatre or going out to dinner with family or a friend.
But – I get it. They are at high risk from COVID. If these kinds of extreme and apparently interminable restrictions are what are required to keep COVID out of our facility then I guess that’s worth it.
Right?
[1] And yes - I know there’s a lot of debate about so-called “long covid,” but IMHO there’s not much to this idea – it seems to be as much a social phenomenon as it is a bona-fide disease entity, and really isn’t anything new given that the possibility of suffering lasting, chronic symptoms after any upper respiratory illness of sufficient severity is something that existed long before COVID, and will exist long afterwards.
[2] (which is interesting, given that we all know now that vaccination doesn’t appear to significantly reduce the likelihood of contracting or transmitting COVID). So – if you’re vaxxed and have COVID – you’re allowed to visit our nursing home!