This gero doc can't take it anymore!
Loneliness is slowly killing nursing-home dwelling older adults.
I’ve been working in long-term care as a geriatrician specialist for going on two decades. The residents at my long-term care facility where I work have been locked-down, isolated, masked, surrounded with masked / muffled / face-shielded staff, had their family members banned from visiting, had volunteers banned from visiting, had their church services cut off, had their paid companion services shut off almost constantly for over two years now - all in the name of virus control.

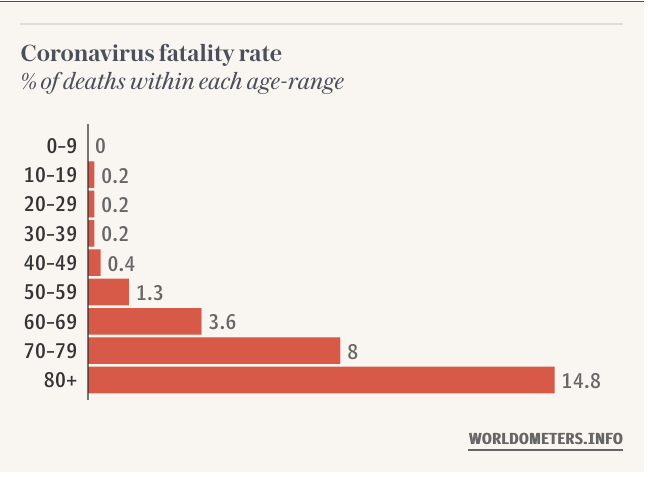
I get it - for the five millionth, billionth time - I get it. You can quibble about the statistics for younger people (and trust me, that’s a whole ‘nother rant of mine) - but for older folks, particularly those in long-term care facilities, COVID has been potentially a very serious illness. We’ve all seen charts like this:
That being said - the population of people I work with are typically at elevated risk for multiple illnesses, chronic and acute - because they are old. This isn’t fatalism, it’s just fact. Worth noting also that being a geriatrician as a clinical specialty is much less focused on life-saving interventions, and much more so on balancing the demands of managing various ailments, illnesses, and challenges of an aging body and mind against the need to continue to live ones life as fully as possible.
“COVID Monomania” in Long Term Care facilities
For *sure* - catching COVID as a 70 or 80 plus year old, particularly those who are by definition at high risk of chronic illnesses (the very illnesses that make one at high risk of COVID complications, like hypertension, diabetes, etc.) puts one at increased risk of, well, dying.
So what have nursing homes in the US done (and worldwide too - but we’ll stay focused on the US for the time being)? Let’s just focus on one of the most important lifelines for residents in nursing homes - visits by family and friends. According to the Centers for Medicare and Medicaid Services, while “visitation should be allowed for all residents at all times,” they are quick to add a whole bunch of provisos to this, namely, visitors must:
remain “physically distanced” at all times (so, no hugs? no kisses?)
remain masked at all times (as I’ve mentioned before - this completely sucks for a population where cognitive, communication, and auditory impairment is rampant)
not be part of a “large gathering” - which means no family reunions! No family barbecues! At my nursing home, that means 10 people or less.
be fully vaccinated or able to pass a COVID rapid test (so, that means no babies or toddlers - SORRY).
On a practical basis, for my nursing home this has also meant that, in order to allow nursing staff the ability to perform the totally distasteful task of policing family visits and making sure everyone is wearing a mask and properly socially distance (which they regularly half-ass or avoid, and I don’t blame them) - we limit our family visits to two hours at a time, and moreover - we require that they inform our social work staff before hand so they can “schedule” them.
In short, it’s pretty horrible.
COVID Lockdown has Smothered Social Connection in Nursing Homes
I can tell you that over the last two years, a handful of spouses of my residents have moved out of the area. On the one hand - for sure, cost of living in the area has gone up, but the strict limitations (and at times, outright bans during times of “outbreak” - e.g., when a case is detected in our staff due to the regular testing that takes place) on visitations have made it so onerous that I suspect that several spouses just don’t see the point of staying in the area.
Others simply don’t show up much anymore, or much less frequently. Sure, they do “visit” with our residents using staff-assisted FaceTime or Zoom calls on their personal devices or the few the staff have - but it’s not the same in so many ways.
Before COVID - in my nursing home we have had localized outbreaks before, mainly influenza, or norovirus. Both, I might add - while normally just a hassle for us younger folks - can be potentially seriously complicating illnesses for older people living in skilled nursing. Typically when outbreaks like that happened we would require staff to mask up, “gown and glove,” we stopped communal dining, and then proceed under these conditions until the outbreak passed. That was just normal.
No longer. Because the idea of “asymptomatic spread” has become so pervasive and such an object of fear or alarm - just because an active outbreak is gone doesn’t mean we don’t “stop with the precautions.”
For example, as I mentioned in my last article / rant - the communal dining hall has been tragically closed in my nursing home for 2+ years now (it’s now basically a storage area, and also houses our “Binax table” where nurses test our asymptomatic staff for COVID on a routine basis). Everyone continues to mask.
Visitation rules I mention above stay in effect. Our nursing home residents can never leave for outings at the mall, restaurant, or movies (or to even go home again - even once).
Regarding asymptomatic transmission - it’s been long-known that one can be an asymptomatic carrier of influenza (also known as seasonal flu) and you can also pass it on to others. So - COVID isn’t special in that regard. I would also venture that asymptomatic transmission is probably something that occurs with any number of viruses and bacteria. But is that a reason to permanently accept forever masking in society - particularly in the case of hearing impaired, communication impaired, and cognitively impaired older adults?
Is the phenomenon of asymptomatic spread a reason to permanently impose social distancing, limit visitations, limit access to the outside, on an open-ended basis?
Meanwhile, life goes on outside, sort of. Mask mandates are still on-again, off again throughout the country (mostly in blue states - states with typically Democratic party, blue-state governance). Everyone who has wanted to get vaccinated for COVID (or boosted - any number of times) can. People are going out to restaurants, movies, and kids are back in school… at least for now.
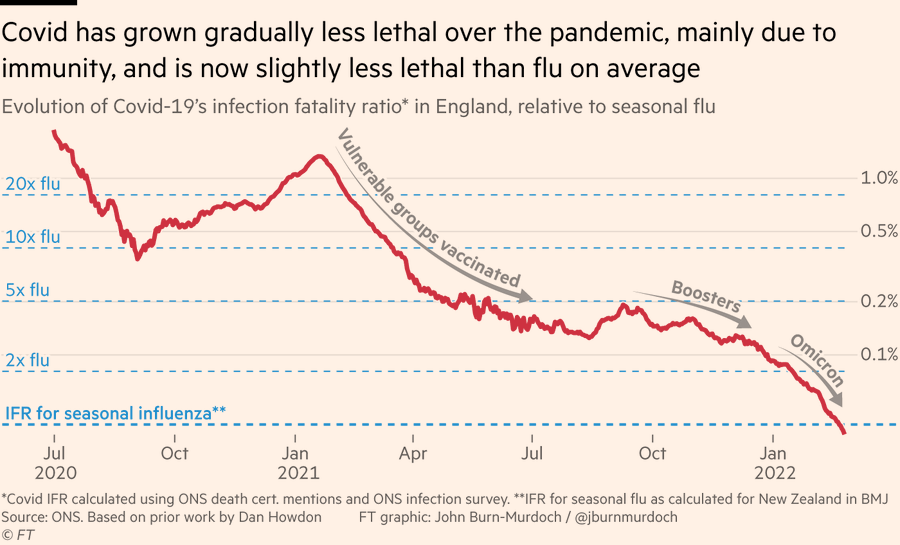
And finally - COVID has simply become less lethal overall. Depending on how you calculate the denominator (important for calculating the infection fatality ratio, or IFR), apparently as of right now has apparently gotten less lethal than the seasonal flu:
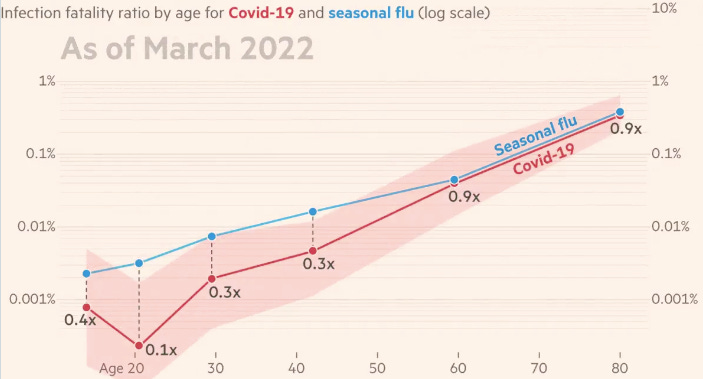
… and the same holds true, apparently, for older adults:
Loneliness Kills.
Loneliness can kill. In a carefully designed 2015 meta-analytic study that looked at the negative health effects of loneliness and isolation across age groups, psychologist Julianne Hold-Lundstadt and colleagues found that the presence of loneliness increased the odds of death by a factor of 26% - and that’s excluding suicide.
Living alone and being objectively socially isolated (both objective indicators of loneliness / isolation) increased odds of death by 29% and 32%, respectively, and supposedly puts loneliness and isolation on a par with smoking 15 cigarettes a day, or being an alcoholic in terms of increasing death risk.
We’re currently into our third year since the ‘stay at home’ (AKA “lockdown”) orders were first issued across the US and that shuttered schools, mandated masks, and devastated businesses. Since then, we’ve clearly had multiple waves of COVID and the disease has clearly become endemic - as in, a disease “regularly found among particular people or in a certain area.” At my nursing home, somewhere around 90% of our residents are vaccinated and multiple-boosted for COVID.
Yet, in my opinion the very measures - these so-called non-pharmaceutical interventions we are relying on to save them from becoming infected - are also slowly killing them.
My Pretty Radical Recommendations
Start acknowledging that the need to address very real, very serious negative health consequences of loneliness and isolation need to be balanced against mitigation of COVID-19 infection risk in older adults - and also that with widespread vaccination and increasingly milder variants circulating - we can now start doing that.
Allow nursing home residents the ability to do congregate dining again. For god’s sake - allow them to eat together again.
Family visitation policies in nursing homes need to go back to being unrestricted. No time limits, and no more having nurses serve as ‘social distance police’ (e.g., hectoring families to not hug or kiss their loved ones).
Lift requirement for visitors to be vaccinated (it doesn’t prevent transmission anyways). Regarding COVID screening, exempt babies and children who can’t comply with COVID screening - it’s more important that older adults see and can interact with their great-grandchildren and the like.
Stop treating older adults as prisoners. Let them leave the facility to see a movie, or go to a restaurant, or visit their home. They are vaccinated. They and their families can wear masks if it makes them feel more comfortable (or not). If infection control types really want to - you can always isolate the older adult to their room for a 7-10 days after they return from their outing.
If a COVID outbreak occurs at the nursing home - treat it like we we used to treat an outbreak of influenza. Have residents stay and dine in their rooms, mask, gown, and glove all clinicians seeing residents, and test test test. Do this until the outbreak has passed. Then allow residents to go back to living lives as social creatures. This is what we used to do before COVID and there’s zero reason we can’t go back to this arrangement.
More than anything - we need to stop treating nursing homes like their highest purpose is avoiding COVID infection in their residents - with every other need being subservient to that. Because that is currently what’s happening. This goes completely against a very powerful concept in geriatric medicine - that of the role of comfort care, or palliation. This is the idea that for older people, particularly those that are infirm and at the end of life (often very typical in nursing home patients) - the emphasis on quality of life is prioritized over life-saving, heroic measures. Often, once the focus is taken off of life-saving measures at all costs (say, in the face of an aggressive cancer or severe heart disease), and the focus shifts to emphasizing comfort and quality of life - miraculously, these older adults often actually live longer.
I think in the case of COVID - particularly given where we are now in the COVID-19 pandemic (e.g., or COVID-19 endemic) - it’s now time to start re-prioritizing comfort and quality of life again. Nursing home residents should no longer live their lives subservient to virus avoidance at all costs. They need to start living their lives again.





I had no family in restricted care facilities during COVID. Once upon a time they were considered nursing homes or assisted living but our federal government and state governors issued executive orders making them prisons AND landing zones for covid positive hospital discharged.
To all of you who have fought for your residents' quality of life and dignity, I truly thank you.